Twenty years ago, if you went to do a blood test for your family doctor - you'd either need to pick up the results from the lab and deliver it yourself to your doctor or if the lab was kind, they'd fax the results to your doctor and your doctor would spend some time to find your paper chart and file the results into your chart.
Today, none of that is necessary. Your family doctor is [most likely] able to view your lab results with just a few mouse clicks. The use of information technology to store and serve your lab results is an example of ehealth. As we find more and more uses of information technology in healthcare, the field of ehealth (or digital health) is born - along with many ehealth-specific professional organizations.
ehealth vs. digital health
Are ehealth and digital health different? No. In fact, the two terms are often used interchangeably. One can find evidence of that in the naming of professional organizations and conferences. In Canada, there's Digital Health Canada, but there's also eHealth Ontario or eHealth Saskatchewan. These organizations share common goals. What's more interesting is that Digital Health Canada is a key host for a conference called eHealth conference meanwhile eHealth Ontario provides Digital Health services.
The term ehealth is part of the "e-" family of terms, that represent the electronic transformation of something - ie. ecommerce, email, etc. It's a convenience term with less syllables to pronounce and is noticeably shorter to write than digital health, digital commerce, or digital mail.
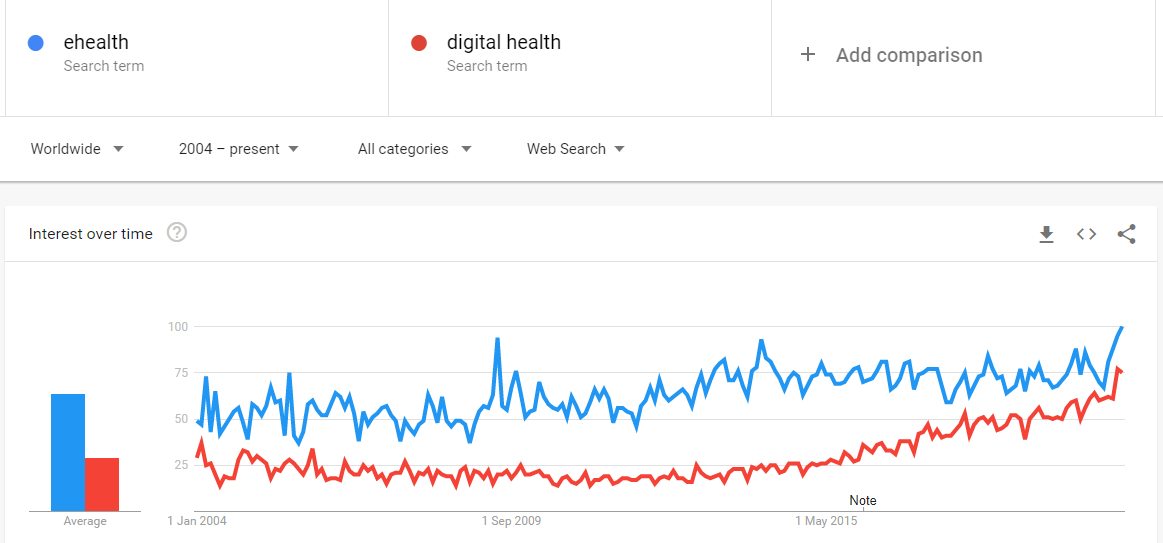
Though the two terms are semantically same, Google Search Trend indicates that ehealth is more popularly used than digital health consistently. Recently however, popularity for the term digital health seems to be growing more than ehealth. For simplicity, the term ehealth will be used for the rest of this article.
Defining ehealth
The term ehealth does not have a widely accepted single definition. As a result, organizations are choosing to define ehealth independently. Unsurprisingly, most will opt to define ehealth in ways that most resembles their own work.
Healthcare Information and Management Systems Society's definition of ehealth focuses on "empowering [patients] to manage [their own] health and wellness ... using digital tools." Meanwhile, the Australian government's definition of ehealth emphasizes on digital technologies that help [connect] points of care. The World Health Organization feels ehealth is more broadly "the use of information and communication technologies for health."
While these definitions appear to be on tangents with each other, they actually do not disagree with each other. In fact, upon closer inspection, we can even infer a commonality among them:
The "health" part of ehealth or digital health refers to the process of care to support or improve wellness rather than the state of an individual's wellness itself.
In other words, for example, the purpose of collecting your blood sugar levels in electronic format does not mean transforming you into something digital - but rather, it is to support the process of delivery of care to you.
More to be done for defining ehealth
Attention and resources given to ehealth is ever increasing. With that, the impact of ehealth has become broader and broader ranging from projects in individual hospitals to global health strategies and policies. Given the critical importance of ehealth, having a consensus definition is paramount, including for the following reasons:
- compare ehealth investment and spending across organizations and countries
- evaluate the effectiveness of various uses of ehealth
- planning, resource allocation, and policy-making for ehealth
While it may be obvious to many that certain activities or technologies must be ehealth - ie. electronic health record - but without a consensus on a shared definition, certain activities or technologies would fall into a grey area in qualifying as ehealth:
- the use of social media for health advice
- web searches for disease, symptoms, and treatment
- self-monitoring technologies for patients
The significance of that is topic for another discussion.
It may be worthy to note that the absence of a shared definition for ehealth does not appear to impede innovation in the field. Today, we take for granted that doctors can look inside of your brain in a matter of minutes without having to lift a scalpel - or that care staff can monitor the rhythm of your heart without physically being at your bedside.
Overall, ehealth is a broad and complex subject thus contributing to the difficulties in achieving a single widely-accepted definition for itself. Without consensus on definition, it will be difficult to evaluate and compare ehealth activities across countries or organizations. Understandably, it will be very difficult to compare certain ehealth activities with each other. Perhaps one solution could be to have a single broad definition for ehealth such as:
ehealth is the use of information technology for the delivery of care or the support of wellbeing.
and then categories of ehealth can be devised (ie. electronic health records, consumer wearables, etc.) for evaluation and comparison purposes. Much like apples and oranges are more broadly defined as fruits, but almost everybody will agree to never compare apples vs. oranges.



